
Key Takeaways:
- Sudden bedwetting, when your child has stayed dry all night for at least 6 months, may be an early sign of juvenile diabetes.
- Juvenile, or type 1 diabetes, is a medical condition where the body does not produce enough insulin. The condition creates excess urine production, which triggers wetting at night.
- Parents often see a combination of symptoms, including sudden bedwetting, increased thirst, frequent urination during the day, weight loss, fatigue, and irritability.
- Diabetes is not the only cause of bedwetting, so talk to your pediatrician for an early and accurate diagnosis.
- Management tools, like organic cotton waterproof mattress pads, make cleanup fast-and-easy when there’s an accident.
Juvenile Diabetes in Children
Juvenile diabetes, also known as type 1 diabetes, is an autoimmune condition where the pancreas produces little or no insulin. Without insulin the body’s cell don’t convert sugar into energy. When sugar builds up in the bloodstream, it can cause life-threatening complications. Diabetes can occur at any age, but type 1 diabetes is one of the most common chronic diseases in children.
Sudden Bedwetting Could be an Early Indicator

Bedwetting, medically known as nocturnal enuresis, is not uncommon in young children. But when an older child who hasn’t had night-time accidents in a long time suddenly starts bedwetting, it’s a sign that warrants attention. The reason diabetes causes wetting is due to the fact that excess sugar in the bloodstream increases urine production. When this excess production overwhelms a child’s bladder, then bedwetting can occur.
When Should You Talk to Your Pediatrician
When bedwetting is coupled with other symptoms like thirst and more frequent urination, then it’s time to talk to your pediatrician. Juvenile diabetes can develop quickly, and early intervention can prevent long-term complications.

Symptoms of juvenile diabetes can include:
- Sudden bedwetting that starts after at least 6 months of dry nights.
- Increased thirst and frequent urination due to the body’s attempt to flush out excess sugar.
- Extreme hunger paired with weight loss, even though your child may be eating more than usual.
- Fatigue and muscle weakness, because the body’s cells aren’t getting the glucose they need for energy.
- Irritability and mood changes that are not typical for your child’s behavior, especially when the irritability resolves quickly after consuming sugar.
Diabetes isn’t the only cause of bedwetting. Your pediatrician can easily diagnose type 1 diabetes with blood and urine tests. Then you can work together on a treatment plan that’s right for your child. Remember that early detection can have a significant impact on positive long-term outcomes.
Managing Your Child’s Condition
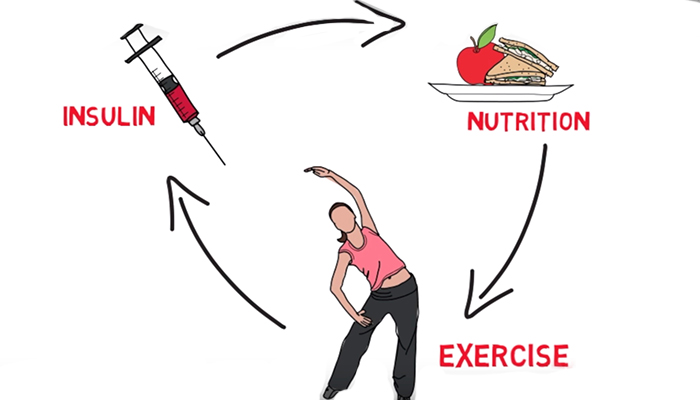
Effective management involves a combination of medical care, monitoring, education, and lifestyle adjustments. It’s important for children to be able to control the negative aspects of the condition while continuing to enjoy a happy childhood with family and friends.

Education and Awareness for Parents and Caregivers
Knowledge is power. Start by educating yourself about every aspect of the condition. Learn how to check blood sugar levels, understand insulin dosage, recognize the signs of high and low blood sugar, and know how to respond appropriately.
Proactively Involve Your Child in the Treatment Process
Empowering your child to take an active role in their treatment can foster independence and build confidence. Teach them about their condition in a way that they can understand and involve them in their daily care routines.

Here are a few steps to involve your child:
-
Explain what diabetes is and the importance of management and treatment.
-
Show them how to check their blood sugar and let them do it under supervision.
-
Include them in decisions about food choices and physical activity.
Remember, your child’s ability to manage their diabetes will improve with practice. And good habits developed early on will provide them with lifelong benefits.
Diet & Exercise Significantly Impact Symptoms
A healthy diet and regular exercise can help stabilize blood sugar levels and reduce the risk of diabetes-related complications.
Encourage a diet rich in fruits, vegetables, whole grains, and lean proteins. Be mindful of carbohydrate intake and teach your child to recognize how different foods affect their blood sugar levels.
Physical exercise can improve insulin sensitivity. Which could reduce your child’s reliance on insulin injections. It’s an outstanding reason to engage in more physical activity, even if your child is more cerebral than physical. And be sure to monitor blood sugar levels before, during, and after exercise to prevent hypoglycemia.
Always talk to your pediatrician about any adjustments to your child’s routine.
Medical Advancements in Diabetes Treatments
Today, the standard medical treatment for type 1 diabetes is insulin therapy, administered through injections or an insulin pump.

However, new medical technologies and medications are being developed on a continuous basis. One recent medical study, conducted by Indiana University School of Medicine in collaboration with the University of Chicago Medicine, was published Cell Reports Medicine (November 2023). Their findings suggest that innovative new type 1 diabetes therapies, with the potential to reduce insulin dependency, could be developed by repurposing the drug α-difluoromethylornithine (DFMO).
Diabetes is an ongoing learning process for you and your child with the goal to maintain a healthy and active lifestyle. Regular check-ups with an endocrinologist who specializes in juvenile diabetes care, in additional to your primary care pediatrician, can help you stay on top of the latest research. And understand which treatments could be right for your child’s individual situation.
Organic Cotton Waterproof Mattress Pads for Diabetes Bedwetting
Consider an organic waterproof mattress pad for diabetes bedwetting. It will protect your child’s mattress from urine leaks, which can lead to bacteria and mold overgrowth. And mattress protectors make cleanup fast-and-easy when there’s an accident.

One of our favorites is MY GREEN MATTRESS. Good Housekeeping awarded this product a Top Choice 2024 Award for Best Organic Waterproof Mattress Protector for Bedwetting. It’s completely waterproof with a breathable, cooling moisture barrier that’s non-toxic. The temperature regulating feature keeps your child comfortable all night long. The construction includes 2 layers of soft GOTS certified organic fiber, which is naturally hypoallergenic and repels dust mites along with other allergens.
MY GREEN MATTRESS has an incredible 4.9 rating out of a potential 5 stars from more than 600 verified customers.
Organic is a good choice for children. The organic certification means there are no toxic pesticides, flame retardants, or chemical waterproofing agents to complicate their medical condition.

Frequently Asked Questions (FAQ)
1. When is bedwetting a sign of juvenile diabetes in children?
Bedwetting becomes a concern when it’s a new pattern, especially in a child who’s been dry for a significant period. If bedwetting is accompanied by other symptoms like excessive thirst, frequent urination, hunger, weight loss, or fatigue, it may be a sign of diabetes and you should talk to your pediatrician right away.
2. Why does juvenile diabetes cause bedwetting in children?
Diabetes can cause bedwetting because the excess sugar in the bloodstream leads to increased urine production, which means your child needs to empty their bladder more often. Increased urine in the bladder can lead to accidents at night when children sleep deeply.
3. Can diet and exercise reduce the risk of bedwetting and diabetes?
While diet and exercise cannot prevent type 1 diabetes, they are critical components in managing the condition. A balanced diet and regular exercise can help stabilize blood sugar levels, which may reduce long-term physical complications as well as bedwetting.
Sources
- Juvenile Diabetes Research Foundation (JDRF). “Type 1 Diabetes Information.”
- American Diabetes Association. “Type 1 Diabetes.”
- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). “Symptoms & Causes of Diabetes.”
- Cell Reports Medicine. “Repurposing α-Difluoromethylornithine (DFMO) for the Treatment of Type 1 Diabetes.”
- Good Housekeeping. “Best Waterproof Mattress Protectors for Bedwetting.”
- My Green Mattress. Product information and customer reviews.
- Mayo Clinic. “Bedwetting (Enuresis) Symptoms and Causes.”

